Cycle 2 of the Fasting Mimicking Diet in a person with Type 1 Diabetes
All material on this website is provided for your information only and may not be construed as medical advice or instruction. No action or inaction should be taken based solely on the contents of this information; instead, readers should consult appropriate health professionals on any matter relating to their health and well-being.
You may want to click over to my first post about the Fasting Mimicking Diet in a person with Type 1 Diabetes to help you better understand this post.
This cycle of the FMD was easier than the first one – and once again I felt better than normal during the fast. In the time that has elapsed since I decided to do this, I did finally track down a Google Group where a couple other Type 1s had engaged in the FMD. I’m excited to see that a couple other people have given this a try and are willing to experiment with their bodies. I’m also a little discouraged because one person reported trying 10 cycles – and during that time, the results were the opposite of what he was trying to achieve. In fact, he wrote me personally saying that after a cycle of the FMD, he went to Indian food and had to dose 200U for a meal that normally would have required 20-30U! Yikes!!
Luckily, this reduced insulin sensitivity does not seem to be permanent, and I do enjoy feeling good during the times of fasting. Non-diabetics may not understand how you could possibly “feel good” during a fast – but basically what you’re doing is removing blood sugar swings from your day. Going from low to high to low blood sugar takes a toll on your body – and when you’re “out of range,” you can feel pretty crappy. In my first two cycles, I found that fasting even enabled me to eat small amounts of carbohydrate without having to inject insulin, which is a nice treat.
As I mentioned in my previous post, I shortened this cycle up a little – down to 96 hours this time. It seems that you start to get the benefits of the FMD once you exceed 48 hours of heavy protein restriction, and 96 hours was a more comfortable duration.
Below is detail of what I ate during this cycle. You will notice that on the 4th day, I began “re-feeding” at dinner time. Calories were quite high. The foods listed were all carefully weighed, but you need to ignore the insulin dosing in these slides because I didn’t record everything (I recorded insulin elsewhere).
- 672 Calories, 8% Carb, 5% Protein, 87% Fat
- 343 Calories, 18% Carb, 5% Protein, 76% Fat
- 558 Calories, 20% Carb, 6% Protein, 74% Fat
- 4266 Calories, 7% Carb, 12% Protein, 81% Fat
Here are my blood glucose reading during the FMD cycle:
A couple observations:
- In this cycle, I didn’t have the very low blood glucose readings that I had on the first cycle. My theory on this is that I had quickly depleted my liver of glycogen on the first day of cycle 1 by doing a big bike ride. In this cycle, I exercised less.
- Insulin still worked fairly well on the day following the fast. Nevertheless, I did need to start increasing the dosage quite a bit in the subsequent days. The mouse study took 50 days and several cycles – so I’m not really expecting any big changes at this point in the experiment.
- In the week following the fast, I was somewhat displeased with my BG control. I wasn’t really making my targets. I had some readings in the 200s as well as a scary 31mg/dL hypo (my worst hypo yet). This is not entirely related to the FMD, but more related to the fact that I wanted to eat some apricots from our tree. My insulin to carb ratio varies dramatically depending on how much I’m moving around – and I was doing some house chores with the insulin for the apricots on board – and suddenly my vision started to black out. To my surprise, this severe hypo was relatively asymptomatic. The lack of suffering during the hypo was kind of a relief – but of course it is quite scary to think that you cannot perceive a hypo coming on. Since then, I’ve had symptomatic hypos when I drop below 60mg/dL – so it seems that my ability to detect them has been restored.
- My average blood glucose and standard deviation deteriorated significantly after coming off the fast. I attribute this at least in part to the fact that I was really hungry post-fast. I suppose that if I had exercised more self-control post FMD, that this wouldn’t have happened. In my head, I figured I would feed “ad libitum” like the mice – which meant eating until I wasn’t hungry any more.
- Perhaps as a consequence of my type 1 diabetes, I am always hungry at all times of the day. This has a reasonable scientific explanation: Type 1 diabetics are lacking at least 3 proteins: Insulin, C-peptide, and Amylin. Amylin is also produced by the beta cells in non-type-1 diabetics. One job of Amylin is to signal satiety.1 since Type 1’s cannot produce this Amylin hormone, it stands to reason that this signal of satiety is also missing. **UPDATE October 30, 2018: I wrote a post about my experience using Symlin, which is synthetic Amylin!
- I am conducting these experiments during the warm summer months in the Northern Hemisphere. We have days here that often exceed 100F, and an added bonus of the FMD is that my body is cooler due to the caloric restriction. In fact, on the warmest nights, I’ve had cool hands and feet and even pulled up the covers in an attempt to stay warm. I can see quite clearly that apart from type 1 diabetes, caloric restriction could be a useful tool in staying comfortable during hot spells.
- This is highly subjective, but I feel like my skin “looked better.” In other words, blemishes and cuts seem to be healing faster. I almost don’t want to mention it because it is so subjective.
- I was in a really good mood during the fast. Also, I felt more “carefree” about things in general. This may have been simply due to having less overall energy – and being less willing to put energy into worrying about things.
- During the fast, my blood pressure drops. It drops very low (approx 90/60). I recently purchase a home blood pressure meter (this one is a good deal), and the results were repeatable during the 2nd (and 3rd) cycle of the FMD. The particularly low blood pressure isn’t very desirable, however, because when I would go to stand up quickly, I had to be careful as to not black out. Once I got moving around, however, things were fine.
***Update 08/15/2018***
My doctor agreed to run a c-peptide test as well as antibody tests (usually these are only run at diagnosis). This was after re-feeding after 2.5 cycles. For the c-peptide, I ate some fruit – and did not dose insulin. The goal was to see just how much insulin my body can produce while stimulated. The result was a mere 0.14 ng/mL. I’ve seen papers where 10 year type 1’s have a higher fasting c-peptide than this… so clearly my diabetes progressed very rapidly. This is probably due to the extremely high GAD antibodies I had. I did note that the IA-2 antibodies decreased by 50%. Since I did not see a benefit from the FMD in my blood sugar management, my insulin dosing, or my test results, I don’t currently have any plans to try again.
***Update 07/24/2018***
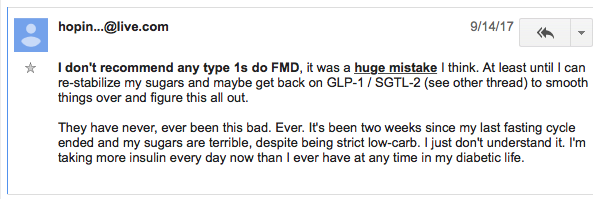
I did start a 3rd cycle of the Fasting Mimicking Diet on the evening of July 16, 2018. By noon on July 18, 2018, I had found a post from Hoping4Cure (another person who has gone through over 10 cycles of the FMD) that read like this:
This post kind of scared me. A few other people had also posted their results in the forum, and many of their experiences mirrored mine – although insulin needs plummeted during the fast, they seemed to be higher during the re-feeding period. Only a few people seem to have done this and reported back – but no one has seen a major reduction in insulin needs – even after completing quite a few more cycles than I have completed. If anything, I get the feeling that blood sugar control is worse afterwards. This was definitely the case with me – as you’re re-feeding, you are basically guessing what your insulin sensitivity is going to be on that hour of that day. If you’re doing the same thing every day, your insulin sensitivity is more stable. If you’re making dramatic switches between fasting and feeding, your insulin sensitivity is all over the map. I hate to be a quitter, but for the time being, I’m pulling the plug on the FMD until I see better results from other people who have tried. When I first began, I believed that I was the first person to have tried this. Now that I see the results from others, I’m going back to what was working best.
What was working best?
If you have Type 1 diabetes, you probably already know that every day is different. I collect a ton of data about my exercise and blood sugars, and then I plot it out in graph form and try to look for patterns. Here is what seems to be keeping me closest to my targets (i.e avoiding uncomfortable swings) AND minimizing my insulin needs:
- Skipping Breakfast. Skipping just breakfast (but not lunch and dinner) is pretty awesome. It is not hard because you still have lunch to look forward to, and you get to skip the morning mealtime dose. This makes morning exercise MUCH EASIER because you don’t get the large variations in blood sugar. Also, your body is primed to burn fat for fuel in the morning, which (as long as you avoid high intensity exercise) seems to result in stable, perfect blood sugars.
- Eating a low and slow carb diet. I do find that with longer exercise, I can “get away” with eating more carbs. I have already started working on a post about this topic, but I think that the reason I can eat more carbs during extended exercise is simply because I have not adjusted my basal insulin appropriately downwards. What I mean to say is that I have to eat more carbs in these instances – which isn’t necessarily a good thing, but I guess you could consider it to be a nice treat. Unfortunately, in these situations, the carb “treat” comes at a time when I’m least likely to be able to get any enjoyment out of the sugar because I’m out of my mind with hypoglycemia.
- Exercise. The best exercise for me seems to NOT be cycling, but instead just puttering around the house. This consists of gardening, and doing household chores. Cycling is second best if I can keep the effort low, long, and consistent. What does NOT work is sitting in front of the computer (i.e. writing these blog posts!)
- Staying Hydrated. I think that the mechanism of action for this might partly have to do with insulin absorption. My theory is that when you’re dehydrated, interstitial fluid is pulled from the subcutaneous area. The problem with that is your insulin is injected into the subcutaneous space (unless you’re doing IM’s2 or using Afrezza3). So, when I’m dehydrated, my blood sugars will creep upwards. It could be that the Lantus isn’t being absorbed as quickly due to the aforementioned reason – or it could be due to my blood becoming more concentrated due to the lack of fluids – or both.
It is not fair of me to say anything about the ACTUAL FMD. The actual FMD is an expensive, clinically tested product (that so far has not been clinically tested on type 1 diabetics). It would be incorrect for anyone to directly associate what I did with their product; they specifically state that their product should not be used by type 1 diabetics. The purpose of this post is to share what happened, and I think the data is pretty interesting: in particular the relatively low glucose readings and reduced insulin dose during the “fast.”
References & Footnotes
- Pancreatic amylin as a centrally acting satiating hormone, Lutz TA, 2005, https://www.ncbi.nlm.nih.gov/pubmed/15777188
- Intramuscular injections – https://en.wikipedia.org/wiki/Intramuscular_injection
- Afrezza is a type of inhaled insulin that works faster than injected insulin. I like it, but it gives me a cough, and may be implicated in higher rates of lung cancer. Furthermore, it is a little more difficult to get a precise (i.e. repeatable) dosage due to the delivery mechanism.
































this was great experiment. real mfd should eat few days only fats nothing else.
and drink water too.. no salt ect..
maybe vitamine for pills if you like..
lantus is bad product.
tresiba insulin is better, atleast i hope it is.
have you rad vertex treatment ?
https://www.vrtx.com/our-science/pipeline/type-1-diabetes/
they heal one patient dm1 for long time possible for good
Yes, it sounds like their VX-880 requires immunosuppressive medications, which is a no-go for many people (including me)… but if the VX-264 does well in evaluation… that is something I would like to pursue!
This was cool to read. I have tried fasting and no carb and both drive me crazy bc if there is even a small re-introduction of carb its all ruined. For example, my kid asks me to have a bite of a cookie she made. I have a comically tiny bite to be polite and I would normally inject 1u (too much even!) and move on, but instead, I spike to 16mmol (over 300) and need 10+ u to bring it down over many hours. Going for walks in the rain to help. Its painfully slow. Anyways for that reason I can not engage in these diets which seem to work beautifully for everyone else. And the weight melts off them. If I hear another podcaster going on about it….. I even tried metformin to see if I could tamp down the liver a bit, but no improvement in the loss of sensitivity or whatever it is. So what works better is low carb (ie Bernstein or just any low amount per meal -15g). It keeps the spikes from being extreme and keeps my body in the mode of using the insulin properly. It is what it is I guess.
I suppose I could stay no carb forever but I can not. I do not like that it is so unforgiving with switching back to carbs.
I am curious if anyone who has had issues with the fastings resulting in higher blood sugars and more insulin needs have ever considered the actual foods they are eating that result in this. Autoimmune diseases are mainly driven by the foods we eat and eating food that you are sensitive to can reverse and make worse anything was achieved from a fasting. For instance, I know I am extremely sensitive to peanuts and almonds. If I eat those, my blood sugar will skyrocket. Same with cow milk and butter. However, after my FMD fasts I do not find any issues with having to increase insulin or having scary high blood sugars, but I also make sure I never eat anything that my body is sensitive too.
Hi Lauren – Thanks for your comment! If one thing is certain with Type 1 Diabetes, it is that we all react differently to different foods. For example, Almonds, Butter, and Peanuts are some of my go-to foods when I don’t want to have a large glucose spike (i.e. they require less insulin for me). Cows milk, however, would be a big spike in my case. That is good to hear that you have been able to resume eating after FMD without having to increase insulin! It’s really intriguing how FMD is different for everyone. If you don’t mind me asking: How many FMD cycles have you done? Have you experienced any overall reductions in insulin needs (or better yet, and increase in your c-peptide?)
I have had the same experience as Lauren with specific foods and that can be different foods for different people… especially ones that are not obvious i.e. non carbohydrate foods. I have not done FMD but did do Whole 30 and felt amazing to the point that I definitely eliminated some foods from my diet.. i.e. specifically hard cheese (cheddar) will make my blood sugar over 300 for 12-18 hours. Knowing this fact alone specific to my body has been huge in controlling my blood sugar and weight. It has not cured my Type 1 Diabetes but has greatly improved glucose control. I will continue to research and jpray that 1 day there is a cure and feel that the food we put in our bodies is KEY to finding the cure.. not the endless medications with immense side effects to continue to make us more reliant on medications and sicker at the same time! No thanks Big Pharma. With my endocrinologist, I have relayed that I will not take any other medications without trying whatever I can naturally first through nutrition and exercise. So after 43 years with Type 1, I am still on just Humalog via insulin pump.
I am curious as to why some type 1’s might become worse after a fast. I have a speculation on the issue. The body in some cases will over promote some functions of the body in order to compensate for the loss of some function, in both normal and non-normal people. Perhaps during a fast gluconeogenesis is promoted more in whatever pathways that the body uses to make it start or continue. The production of amylin is one of protein associated with gluconeogenesis and when eating it is released to suppress gluconeogenesis for some amount of time. Of course, type 1 diabetics do not produce amylin, but could some other pathway in a type 1 diabetic be promoted in order to maintain energy? Are the same pathways being promoted in normal people when they fast? I would be curious to get a blood test of a normal person before and after a fast to see if amylin levels change with a given macronutrient meal. Perhaps the production of amylin is suppressed in a normal person for some amount of time so that the body will undergo gluconeogenesis more often. Perhaps whatever pathways that activate gluconeogenesis are promoted in both normal people and type 1 diabetics. In normal people these changes may not be apparent as they would release more insulin when sensing higher blood sugars from the release of glycogen and glucagon. The body may be reacting to a time of “deficit” and perhaps in our evolutionary history individuals that would have an extended time of gluconeogenesis would be able to gain greater energy stores for what might be just a one time meal or couple of days meal. Also, with increasing gluconeogenesis the body will want to release more insulin to shuttle the nutrients and fat to be stored for a possible reoccurrence of a fasting state. For type 1 diabetics this may be bad as we will have to increase our insulin doses to combat this time of increased gluconeogenesis.
Thanks for sharing your experience Brian. I am considering to start a series of water fast cycles and your sharing is very helpfull. I think that the increased use/need for insuline in the days after breaking the fast is only natural – you should probably feast in order to rebuild whatever the autophagy cleared out of your system – including rebuilding b-cells, maybe not restrict yourself in this phase. On the subject of exercise I have read that cell permeability increases when doing hard or prolonged exercise and therfore will offer more use of glucose for less insulin. Probably this is the reason for your low bs on trial 1. Antibodies is said to be reduced hard as soon as normal bs is acheived, ref dr Bernstein. The key might be gad as people like me with low gad(lada) , <90 seem to maintain (and hopefully restore) more easily. I'm on the Bernstein protocol since 2,5 years and only use an avrg of 6u bolus/day.
I hope you keep up the good work, trails and sharings, regards Tom
Hope to
Thanks for sharing this information. It’s extremely interesting.
I’ve been reading as much as I can about diabetes since my 8 year old daughter was diagnosed with T1D two weeks ago. I’ve also been deeply fascinated with the benefits of fasting ever since I saw the documentary “Science of Fasting” some years ago. That made me look into if fasting would have any positive effects on T1D, and that lead me to Walter Longo’s research and this blog.
I think the research on fasting and T1D looks very interesting. But I suspect that there might be one big problem. It looks to me like there is increasing evidence that T1D is associated with a persistent enterovirus infection in the pancreatic cells as well as the gut mucosa. If this virus infection persists, newly formed pancreatic cells will probably quickly also be infected and targeted by the immune system. It looks to me like eradicating the virus completely might be very difficult. They are doing a study in Norway and Denmark now where they are testing giving two antiviral drugs for 6 months to children with newly diagnosed T1D. The results will come at the end of this year, or early next year. I’m optimistic that this will show some effect in slowing the virus infection and prolonging the honeymoon phase. I of course hope that they will be able to stop the progress of the disease entirely, but I think that that would be highly unlikely.
I speculate that if one was able to eradicate the virus, one could use fasting to make the pancreas heal. I think fasting has shown some specular results on several conditions, but I’ve seen no evidence that it helps at all when it comes to viral infections. Quite on the contrary, I think it looks like the evidence points to that it can actually make it worse.
I really hope they figure out this soon, and will be able to fix this disease.
Rune – Thank you for the great insight. I agree with you that some research on T1D has suggested that T1D is caused by Enteroviruses (or maybe Rubella or Coxsackievirus B or Rotavirus or Cytomegalovirus)… This hasn’t been conclusively proven, except in the case of congenital rubella syndrome. One aspect I question about the virus theory is the fact that T1D hasn’t been shown to be contagious – yet viruses are contagious. Regardless, the virus-etiology theory makes a lot of sense to me because it would help explain why the immune system is attacking these cells. Like you, I’m optimistic that this can be figured out… and possibly soon given the rapid advances we saw in vaccine technology in the last year. With regard to your daughter, I’m sorry to hear that. One thing I do know is that many people have prolonged the honeymoon period by jumping right into excellent blood sugar control at the appearance of T1D. From what I have read, the honeymoon period isn’t always easier, but it might be beneficial to keep the beta cells working as long as possible because they produce 2 other important hormones that are not normally being replaced in standard T1d treatment (Amylin and c-peptide). I’m not a big proponent of fasting because it didn’t work for me – and to my knowledge, it hasn’t helped any other T1d’s significantly increase their insulin production. The worst part, however, is that you tend to overeat when you do start re-feeding which guarantees massive swings. T1d is much easier to manage with a slower and steady input of food. Worth noting, Longo has been reticent about the use of the FMD in T1D; their mouse model of T1D does not feature the ongoing beta cell attack. I’ve also uncovered some additional flaws in the way they chose to interpret the data (this merits its own blog post). Sorry to be so down on FMD! So far after a lot of self-experimentation, the ways I have managed to feel the closest to normal are: Very careful insulin control, pre-bolusing for meals, planning around exercise, and eating (relatively) low carb meals. Thanks again for writing!
Thanks for replying, Brian. I love hearing your thoughts, as you’re obviously both very knowledgeable about these matters and intelligent. I’ll continue following your blog in the future.
I think this article sums up much of the current research into enteroviruses and T1D: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6294842/
The drugs they are testing giving to newly diagnosed children in Norway and Denmark are Plecanoril (which is not yet approved either in USA or Europe, but which has been shown effective against this type of infection in several studies: https://www.researchgate.net/publication/6563021_Antiviral_treatment_of_Coxsackie_B_virus_infection_in_human_pancreatic_islets ) and Ribavirin (which is a more common drug that are used to treat other viral diseases, and also has been shown effective against this type of infection: https://pubmed.ncbi.nlm.nih.gov/31705692/). By the end of this year they will know who has gotten placebo and who has gotten the antiviral drugs, so then they can probably conclude once and for all if the virus is to blame.
When I posted a question in a Norwegian diabetes Facebook group, asking if anyone had children participating in this study, and what their experiences were, I got a lot of responses. People was telling me that their child still could produce quite an amount of insulin 2,5 years after the diagnosis. It’s obviously too early to conclude if this is because of the drugs, but also doctors who have access to the preliminary data, tells me that they think it looks like the treatment probably has some effect in prolonging the honeymoon phase.
When it comes to regulating my daughters blood glucose levels, we find that very difficult now in the beginning. We’ll hopefully get better at it soon, but still her levels are either too high or on it’s way to become too low about half of the time. It’s very interesting to read how you’re able to do several ultra endurance sports with T1D. Our daughter is used to being quite active, but now her blood glucose levels drops very rapidly when she is active, so it has become a lot more complicated. But we’ll hopefully figure out how to manage this better soon.
This is Fantastic Brian. Thank you for taking the time to share this! My 15yr old son was diagnosed 14 months ago and through another endeavor I met Dr Longo at a conference. I am tracking Fasting closely. Your observations are very helpful. I will have my son read through all of your T1D blogs.
Hello,
Thanks for this post. I found this paper showing some foods activate the autoantibodies:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5551512/
One of the foods that does that is apricots and even some types of fish. Perhaps you might want to try this again only this time avoid the foods on this list and see how it goes? Also, your dietary snapshots are a little small to read. Could you post bigger photos? Thanks
Hello,
Thanks for this post. I did some research and found this:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5551512/
There are some foods that activate the autoantibodies that cause Type 1 Diabetes and apricots is one of them as are some other foods I think you were eating during the refeeding phase. What would be interesting is if you tried this again for a number of cycles then when you refed you steadfasting avoided all of the foods that are on that list so that you don’t kill them off again.
Hello I have done more than 16 cycles of FMD, I am type one, like you. My overall conclusions is that you do get insulin production after a fast, but, after you stop it all goes back to usual, the auto-imune reaction kills what ever you gained. As for major insulin resistance, the way I deal with it is the first day, stay away from carbs, re-introduce them slowly. And I do long runs and usually in one or two days things are back to normal.
Feel free to contact me if you have any questions
Best
Nicolas
Nicolas – Thanks for writing in with your experience! It is very helpful to have a report from someone with T1D who has more experience with the FMD than I do. I cannot prove that I had insulin production just after the fast because I didn’t do a c-peptide immediately afterward. Several days after the last cycle in the “rebuild phase,” I did do a STIMULATED c-peptide (i.e. I ate some apricots without dosing insulin ~90 minutes prior to my blood draw). My c-pep was 0.14mg/dL (0.0464 nmol/L) which is VERY low even for fasting (non stimulated). My insulin production is depressingly low considering the “short” duration that I’ve had diabetes. Thanks for your advice about re-introducing carbs slowly. I’m curious: do you plan to continue to do cycles of the FMD? In my case, I seem to have fewer fluctuations when just sticking to a regular schedule of eating. I’m curious to know what benefits you are experiencing from the FMD, which may renew my interest (or the interest others reading this blog).