Symlin for use in Type 1 Diabetes
All material on this website is provided for your information only and may not be construed as medical advice or instruction. No action or inaction should be taken based solely on the contents of this information; instead, readers should consult appropriate health professionals on any matter relating to their health and well-being.
Amylin – The other missing hormone
When you think of type 1 diabetes, probably the first word that comes to mind is “insulin.” When you have type 1 diabetes, your immune system has destroyed the cells in your pancreas that produce insulin – but insulin is not the only hormone that used to be produced by these cells. The other hormone is Amylin. In spite of the fact that type 1 diabetics1 are actually missing TWO hormones, insulin gets all of the attention, and amylin is generally ignored. Why? Because a person can only survive a few days without any insulin in their body (and only a few hours under certain conditions). This is very noticeable. Conversely, a person can survive for decades without any amylin.2. But what happens to your body without this hormone?
In a person with a functioning pancreas, amylin is co-secreted with insulin – this usually happens when you eat. There are at least 3 things that amylin does in your body:
- Amylin signals satiety. This makes sense – if you’ve eaten, your body needs a signal to stop eating.
- Amylin tells your liver to slow down sugar production by your liver. This makes sense too because if you’re eating food, you’re adding fuel to your body. You don’t need to produce sugars while you’re eating them!
- Amylin slows down the movement of food out of your stomach.
If you have a functioning pancreas, you may take these 3 activities for granted because they all happen automatically without you thinking. If you’re a type 1 diabetic, having these functions restored can lead to a MAJOR improvement in how you feel daily. Now that you know what amylin is – and that as a type 1 diabetic, you’re missing your amylin, let’s talk about how you can get it back!
Symlin – The man-made version of Amylin
I first learned about Symlin in Dr. Bernstein’s Diabetes Solution Book. He only dedicated a page to the topic. Similarly, my other favorite book (Think Like a Pancreas) only devotes a few pages on how to get started using Symlin. In “Think Like a Pancreas,” Gary Scheiner definitely acknowledges the benefits of replacing this hormone – but also mentions that it is very difficult to learn how to time and titrate the dose. He also pointed out that people don’t like to take extra injections.
Here were my thoughts on the topic:
- I don’t like taking “drugs,” but I don’t consider this to be a drug because just like insulin, my body should be making this – and it isn’t. Everyone else has this hormone in their body.3
- I don’t mind extra injections – especially if they can improve my life.
- I enjoy the process of experimentation, keeping records, and comparing results.
- Before diving in, I decided to do some independent research and found this AMAZING 3-part guide/resource on how to start using Symlin.456 I don’t see the need to re-invent the wheel. If you’re going to try Symlin, use the links to the 3-part guide provided here or in my footnotes.
I asked my doctor for a prescription. Like most doctors, she had never heard of Symlin. It’s not like they advertise medicine for type 1 on TV – all that stuff is for type 2 diabetes! She did some reading while I was there and finally said, “Oh, I should prescribe this to some of my type 2 patients!” It probably won’t benefit early type 2 diabetes (but end-stage type 2 diabetics could probably get the same benefits as a type 1 – though they may need a higher dose). After some wrangling with my insurance company, I finally gave up on getting this very expensive medicine covered. Then one day – out of nowhere – I got a call that my prescription was ready – and at a reasonable co-payment… so I hurried to the pharmacy to give it a try!
Symlin – What it feels like
For years, I have been hungry all of the time. By this, I mean nearly 24 hours a day I feel like I am starving. Before I knew I had type 1 diabetes, I attributed this constant hunger to my exercise. In the past, I would go to dinner with my friends. I’d eat my own meal, and then clear all the leftovers from everyone else’s plate. Then, when I got home, I’d grumble about the “tiny restaurant portions” and have my “real dinner” which was so big that it usually contained 2 or 3 times the calories of my original dinner and scavenging from friends’ plates. Even after eating all this, my stomach felt physically “stuffed,” but I was still hungry. Back then, I used to use foods like ice cream to “fill in the gaps.” It seemed like ice cream might help trigger some sense of satiation without causing my stomach to burst. I used to figure that the reason I did not gain weight after eating so much food was because I exercised a lot. It wasn’t until I discovered that I had type 1 diabetes that I realized the reason I did not gain weight was because my pancreas wasn’t making enough insulin!7 When there isn’t enough insulin in your body, the food you eat cannot get into your muscles and your fat. Instead, it pools up in your blood and eventually gets excreted in urine. Over time, there is so much energy pooled up that you are peeing constantly just to get rid of the energy (in the form of sugar) because it has nowhere else to go. Once I started using insulin, I could no longer “pee out” my food. It started sticking to me, and in a week and a half, I ballooned from 160 lbs to 185 lbs because suddenly all of the food I was eating was getting into my muscles and fat like it was supposed to. The problem was that I was still always hungry! I had to use 24hour per day will power to avoid gaining weight now – all this because my body was still not getting the signal that it had enough to eat. Now that I was on insulin, I would eat enormous low-calorie salads to physically fill my stomach without gaining weight. I would be stuffed – but hungry.
For 14 years, I was also having stomach issues – a near constant dull ache in my abdomen. A lot of time and research went into identifying the cause of this pain. Could it have been that there was too much food in my stomach, and this excessive amount of food was entering the small intestine too quickly due to a lack of the hormone amylin? I’m still waiting to be sure, but (fingers crossed), I haven’t had the pain once since beginning Symlin.
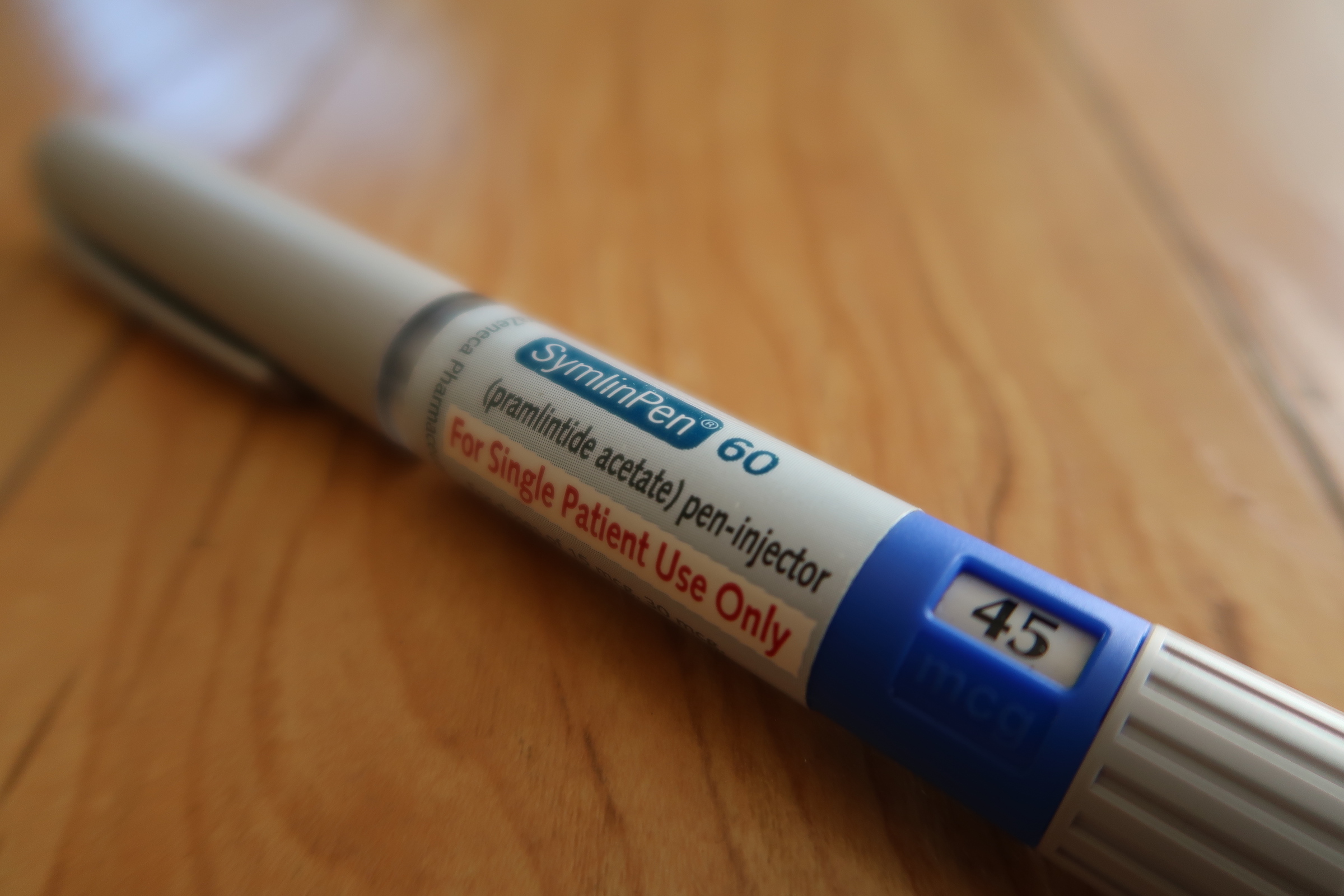
I followed the instructions on how to begin titrating the Symlin dose. I started with the 15U, recommended for type 1 diabetics, and “thought I felt something” (which usually means placebo effect!) I did several days stopping at each dose – 15U, 30U, 45U. I definitely felt something when I got to 30U.. nausea. That was to be expected. I continued with 30U for a week, and I have eventually stopped at 45U. The typical dose for a type 1 diabetic is 60U, but I am completely pleased with the effects of 45U. I try to take the injection about 10 minutes before I start eating. After I take the injection, I set a timer for 30 minutes, wait 10 minutes and start eating. When the timer goes off, it has been 20 minutes since I started eating, and 30 minutes since Symlin. At this time, I take a blood glucose reading and evaluate how much insulin I’m going to inject. Usually at this point, my blood glucose is a happy 80 something!?! I then take a reduced meal-time insulin dose that is about 60%-70% of what I had been taking before. I will set another timer for 80-90 minutes to check in and make any insulin / glucose tablet corrections as needed.
Around the 20-30 minute mark is when the magic happens.
Get ready to start feeling like a normal person again!
If you’re not a type 1, you will probably never understand the magnitude of this ecstatic feeling. I was full – but not stuffed. Having this peaceful, comforting feeling of satiation was amazing – and new. I was not constantly on edge thinking about the next meal. I can now think about having a snack and easily say, “nah, I can wait until the next meal.” This feeling of satiation is improving other areas of my life. I feel more relaxed and happy. Also, by taking smaller doses of insulin, I’m less susceptible to hypoglycemia (I haven’t had a bad one in 3 weeks – previously, I’d have a nasty hypo a couple times a week). In fact, with a small all-protein-fat-fiber meal (i.e. zero carb), I will sometimes skip the insulin all together – and just rely on Symlin’s ability to reduce the liver’s production of glucose combined with my basal (long acting) insulin! This feels great, and I can agree to unscheduled exercise without worry! This is huge for me because I often have unanticipated exercise. An activity as simple as gardening after a meal can send me plummeting and feeling awful for 20-30 minutes.
Symlin – Improvements in Blood Glucose
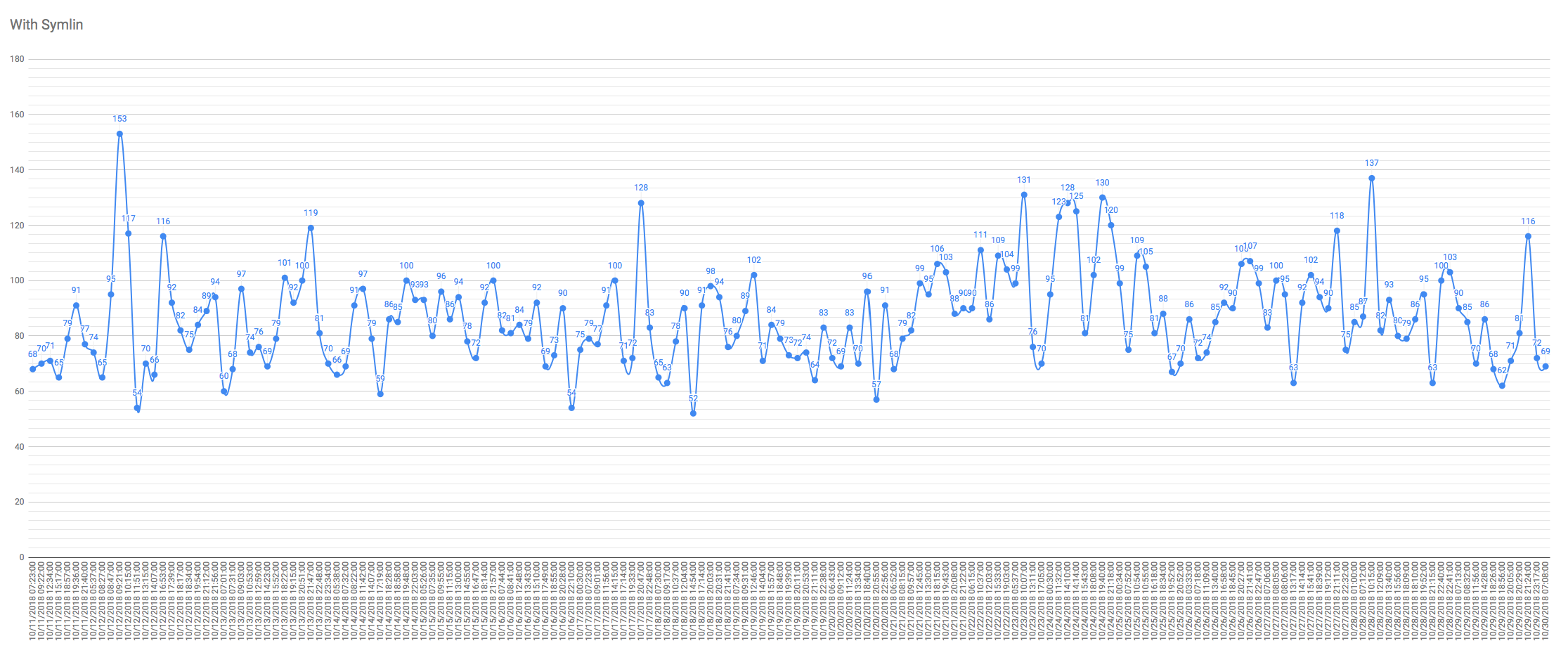
My blood glucose readings while on Symlin. Lest you think these numbers are attributable to the “honeymoon stage,” note that my pancreas produces almost zero insulin. This is almost entirely being controlled manually. My last c-peptide test was a “stimulated” (i.e. I ate a bunch of sugar without taking insulin 90 minute prior to the test). The result was 0.14 ng/mL (that’s 0.0464 nmol/L for the Euro folks).
I’ve been so focused on how good this hormone replacement is making me feel, I nearly forgot about the other big improvement: better numbers! I made a graph of my data from the last 10 days. By combining Symlin with what I have already learned about nutrition, I’m consistently achieving numbers that are in the non-diabetic range. As my experiments become habit, I find that living with type 1 diabetes is getting easier. I hope this post helps you if you’re a type 1 or just curios about how beta cell hormones work in the human body. I’m not providing any medical advice here, but I do encourage you to read the 3-part series linked below if you’re going to give it a try yourself.
References & Footnotes
- Note: And people who have had their pancreases surgically removed
- Note: As a side note, an area of research worth following is Amylin’s involvement in amyloid plaques and dementia – is there a connection?. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4068803/
- Note: Whenever I mention Symlin to non-diabetics, they often reply, “Oh, well I don’t like to take drugs.” My point is that people with Type 1 diabetes (and people who have had their pancreases removed) do not make this hormone. I don’t consider this a drug, but replacement of a hormone that we ought to have in our bodies.
- Reference: A Practical Symlin Guide for Type 1 Diabetics – Part 1: Introduction
- Reference: A Practical Symlin Guide for Type 1 Diabetics – Part 2: Acclimation, Meal Boluses, and Hypoglycemia
- Reference: A Practical Symlin Guide for Type 1 Diabetics – Part 3: Advanced Techniques, Train Wrecks & Disasters, and High Protein/Lo-Carb Diets
- Note: Many people don’t understand this because they associate “diabetes” with being overweight. That is often the case in type 2 diabetes which begins with the pancreas producing TOO MUCH insulin. Conversely, in type 1 diabetes, the person does not make much or any insulin. Insulin is required to store food energy in muscles and fat, so if you don’t make enough insulin, you literally starve to death as the food you eat passes out your pee.



























Great site that ms for sharing. Are you still using Amylin? I’m also curious if you’ve ever experimented with GLP1 agonists. Easy to get and offers similar satiating results—maybe too much in my experience. I’ve using R over the faster insulins better matches the curves though.
Hi Mike – Thank you for writing and for your excellent questions and comments. I have been meaning to write a follow-up post about Symlin, but in a nutshell, it behaves a little differently than it did when I first started and published this post. I had to titrate up the dose a bit, and it works best if I cycle it (in other words use less for a few days, then go back to using more). I’ve capped my usage at 60mcg per meal. The satiation effect lasts for about 2-3 hours, and I’ll have zero interest in food during that time. The problem with that is if I take it before a 6PM dinner, I won’t eat enough, and then find the hunger returning around 9pm… not a good time to be hungry! So, it isn’t perfect, but I like it enough to continue using. Thank you for mentioning GLP-1 agonists. I’ve been intrigued by this for a long time – I even had a sample of Trulicity in my possession at one point. I didn’t use it because it is a once-weekly injection – meaning that it persists in your body for a long time. My fear was that with exercise, I would have serious lows. One of the mechanisms of action of GLP-1 is to inhibit inappropriate post-meal glucagon release – but you really need glucagon when you’re exercising. Is is challenging to get GLP1 as a Type 1? Supposedly it is off-label for T1d, though I have read a lot of reports of T1’s benefitting from it. Apparently >65% of long term type 1s have some residual beta cell function ( https://diabetes.diabetesjournals.org/content/59/11/2846 ). Note that in the conclusion of this paper, they suggest that “stimuli to enhance endogenous β cells could be a viable therapeutic approach in a significant number of patients with type 1 diabetes, even for those with chronic duration”. GLP-1’s main mechanism of action is to stimulate glucose-dependent insulin release from the pancreatic islets… so it is definitely promising! The question is: how to get your insurance to cover it if you’re “only” a T1?