Cycle 1 of the Fasting Mimicking Diet in a person with Type 1 Diabetes
Before reading any further, please know that this blog does not constitute medical advice. My plan is to outline my own experiences in managing type 1 diabetes in the hopes that I can provide interesting and educational information for my readers. I do not recommend that you try to emulate any of the experiments that are discussed on this blog.
Introduction
I have been living with type 1 diabetes since September 2016. In this post, I plan to discuss an ongoing self-experiment to see if there are ways I can help myself feel better more often, avoid dangerous hypoglycemia as much as possible, and exercise more safely and enjoyably. The duration of my type 1 diabetes is important to state in this post because patients sometimes experience a “honeymoon” period in which the person with type 1 diabetes requires less insulin before the diabetes becomes “full blown”. During this time, the ailing pancreas is still sputtering – doing a little bit to help out – giving its last gasp as it is finally killed off by the immune system. This honeymoon period has been documented to last anywhere from a couple days to up to a year – in very rare cases, longer. Every person is different, and without careful, stimulated c-peptide testing it is difficult to discern if the pancreas has made any sort of a comeback. By the time type 1 diabetes is usually diagnosed, about 90% of the insulin producing cells have been killed.
It is also important to discuss disease duration because I have seen a couple people post that they cured their own type 1 diabetes – only to either vanish from the internet or resume taking insulin injections after a brief remission. In one amazing case, a blogger named Caroline Potter 1 reported that she temporarily stopped using insulin for 2.5 years by making dietary changes. This is extremely rare, but two and a half years without insulin is a fantastic improvement in the quality of life for a type 1 diabetic! There are other people who are experimenting with dietary changes and nutritional supplement “cocktails” 2 trying to further this period of remission. Because Type 1 diabetes is different in everyone, surely not everyone will be so fortunate, but this blog is where I’d like to start documenting and share my own experimentation in this realm. Even before I began this experiment, I’ve been fine tuning my management and feeling better more often – and in the process using less insulin. Except for occasional experiments, I’m very strict about not letting my blood sugar exceed 110mg/dL. This won’t be a situation where I’m using less insulin, but allowing myself to run higher blood sugars.
Are you just hungry for the data? Click here to skip to it.
My Diagnois
In September 2016, I presented with all the classic symptoms of type 1 diabetes. I had lost 10 pounds in 1 week, and was heading to the bathroom every hour (yes, that’s 8 times per night). Over the next few days, I had several tests, including antibody tests (intentionally tested just prior to my first insulin injection). I wanted to get a baseline. Here are my results:
| Test | Result | Normal |
|---|---|---|
| A1c | 11.9% | 4.2%-5.6% |
| Fasting Blood Sugar | 290 mg/dL | 70-100mg/dL |
| c-peptide | 0.5 ng/mL (low)3 | 1.0-5.0 ng/mL |
| Insulin Ab | <0.4 U/mL (negative) | <0.4U/mL |
| GAD Ab | >250 U/mL (strongly positive) | <5.0U/mL |
| IA-2 Ab | 3.6 U/mL (positive) | <0.8U/mL |
| Zn Transporter 8 Ab | <10 U/mL (negative) | <15U/mL |
Differentiating between the types of diabetes is not a black-and-white science. For example, about 10% of people with type 2 diabetes can present with one (but usually not two) of the antibodies 3. Usually having 2 or more of the antibodies confirms a type 1 diagnosis with certainty. Furthermore, 19% of type 1 diabetes cases present with neither of the 2 main type 1 antibodies (GAD and IA-2)! 4 In my case 2 of the 4 antibodies that are normally examined came up positive. In fact, GAD Antibodies were beyond the measurable scale at my lab. Combined with the very low c-peptide, this looks like classic type 1 diabetes.
As a secondary test, we can look at some of the markers that would be suggestive of metabolic syndrome, which is what we often call type 2 diabetes. I want to rule that out as a possibility, because type 2 diabetes often responds very well to dietary changes. (This lipid panel below is from after I got my blood sugars controlled by insulin injections. I requested it because I had begun eating a diet that was comprised of 80% fat, 5% carbohydrate, and 15% protein and was worried about high cholesterol):
| Test | Result |
|---|---|
| Cholesterol | 178 mg/dL |
| Triglycerides | 54 mg/dL |
| HDL | 95 mg/dL |
| LDL | 72 mg/dL |
| Cholest/HDL Ratio | 1.87 |
| Triglyceride/HDL Ratio | 0.6 |
The Triglyceride to HDL ratio is an indirect measure of insulin resistance 5 (insulin resistance is the hallmark of type 2 diabetes). Having a level less than 2.0 suggests insulin sensitivity (i.e. NOT type 2 diabetes). My result of 0.6 is FAR below average, and could be considered the antithesis of type 2 diabetes – suggesting very high insulin sensitivity, and most likely NOT type 2 diabetes.
Based on these results, I believe it is safe to conclude that I have some form of type 1 diabetes (type 1 is the autoimmune form of diabetes). Within type 1 diabetes, however, there can still be some variation. Nevertheless, with the presence of auto-antibodies, the general prognosis is that the pancreas will eventually lose complete function (if it hasn’t already). At the time of diagnosis, the pancreas has usually lost 90% of its beta cells, and the disease usually progresses to 99% destruction shortly afterward. Wanting to preserve that function as much as possible, I began the Dr. Bernstein Diet immediately after diagnosis. Although my management has not been perfect, it has been very good – and I attribute this largely to following the protocol outline in his book. I’ve read it twice and plan to read it again!
What have I been eating up until now?
Below is an image gallery that gives a very rough idea of what I’ve been eating in my implementation of the Dr. Bernstein Diet prior to the fasting. These are some slides that I made a year ago, and they are illustrated with results from my Dexcom G5 as well as myfitnesspal. This is just an example of what I was eating; these are from 1 year ago, and I’ve made some slight modifications to the composition of my diet since then.
- 77% Fat, 18% Protein, 5% Net Carb. As you can see from the Dexcom, I may have injected slightly too much Novolog for this meal, but it resulted in fairly stable blood glucose for the day.
- 80% Fat, 15% Protein, 4% Carb. Again, a very stable meal.
- 81% Fat, 12% Protein, 7% Carb
- 60% Fat, 35% Protein, 5% Carb
Why bother optimizing?
Doctors and critics will assert that all type 1 diabetics need exogenous (injected) insulin for life. I’m not here to argue that. In fact, in conducting this experiment, I don’t have any plans to stop using insulin all together. My goal is improved management of my blood glucose and reduction of symptomatic hypoglycemia. If you have type 1 diabetes, you are familiar with the significant morbidity caused by having to dose insulin. Non-diabetics often think that the worst part of type 1 diabetes is having to administer injections. In reality, injecting is the most minor component – if all I had to do was take 10 daily injections that managed my disease, I probably wouldn’t be looking for a better solution – I’d just take my medicine and shut up. Thanks to modern needles, injections do not hurt, and thanks to insulin pens, delivery is facile.6 The major problem is calculating the dosage. There are dozens of insulins, and I use three (a long acting called Lantus that lasts 24 hours, a short acting called Humalog that lasts about 4 hours, and a short acting called Novolog that lasts 3 hours). One big problem is that sometimes in sport, I sometimes need my insulin to last just 15 minutes (for a sprint in a bike race, for example)… but once you inject an insulin that lasts 3 hours, you cannot remove it. So, in a race effort, I have no safe way to bring down my blood sugar. As a result, if I go hard, I end up riding around for the next two hours with syrupy, acidic blood, which is neither good for my health nor my performance. If I could take an insulin that started working instantly, and went away in 15 minutes, I could sprint and then recover.
That’s just one example, but the consequence of any mis-calculation in insulin is either a bout of hypoglycemia or hyperglycemia. The best case scenario for hypoglycemia is feeling awful. The worst case is hospitalization or death. I’ve spent enough 20 minute sessions convulsing on the side of the road or on the floor to know that this is something I want to avoid at all costs. With regular diabetes treatment, I deal with this risk every time I put something in my mouth, every time I exercise, and every time I go to sleep, and sometimes during my sleep. That’s most of the 24 hour day. THAT is the challenge of type 1 diabetes, and the one that I have the goal of improving.
How can I improve over the Dr. Bernstein Diet?
Utilizing the Dr. Bernstein Diet, frequent testing (about 10x per day), and frequent insulin injections (I’ll often correct 1U at a time as opposed to over-bolusing), I have managed to maintain an A1c in the non-diabetic range. For many, that would be satisfactory, however, I still see room for improvement and I enjoy experimentation. As I have learned how to time my eating, strategically dose insulin (making careful allowances for exercise), you can see that my results have improved.
| Date | A1c | Average Daily Lantus | Average Daily Rapid (Humalog/Novolog) | Average TDD (Total Daily Dose) |
|---|---|---|---|---|
| 2016-09-28 | 11.9% | 0U | 0U | 0U |
| 2017-01-06 | 5.2% | 8.9U | 0U | 8.9U |
| 2017-05-08 | 5.4% | 11.9U | 1.6U | 13.5U |
| 2017-07-18 | 5.6%8 | 16.3U | 9.6U | 25.9U |
| 2017-11-03 | 4.8% | 15U | 4.6U | 19.6U |
| 2018-03-13 | 4.8% | 13.5U | 3.8U | 17.3U |
For reference, an A1c of 5.6% or less is considered to be within the non-diabetic range. Strict adherence to the Dr. Bernstein Diabetes Solution has worked well for me! My TDD (Total Daily Dose) is now a little less than average for a person of my weight. This is probably due to the low carb diet and an above average amount of time spent exercising (sometimes 5-8 hours per day).
But Type 1 diabetes cannot be cured!
I have seen posts where people claim to have cured their type 1 diabetes, but the truth is that a spontaneous “cure” is very, very rare. It is important to remember that it is not impossible.7 It is also important for us to study the very few cases of true remission in order to learn how to better help people suffering from this disease. Whenever you mention “cure” and “type 1 diabetes” in a blog, there is a huge risk of drawing anger from diabetics. For example, I read a poignant comment concerning diet in the treatment of type 1: “Would you suggest to a parent, with an exclusively breastfed, 10 month old baby with Type 1 diabetes, that they should change his diet and wean him off insulin?” The answer is of course, NO! It’s important to remember that this blog is just to recount my own experimentation, and it is not advice. It’s also important to remember that Type 1 diabetes manifests itself differently in each individual.
Warnings, Risks, Dangers
Long standing advice from the American Diabetes Association is that type 1 diabetics need to eat a high carbohydrate diet. This has slightly changed in recent years in favor of a more sLOW carb approach. Other medical advice given to type 1 diabetics is that you need to correct any blood sugar below 70mg/dL. Also, standard advice is that you’re doing well if your post-meal blood sugar stays under 180mg/dL. Fasting is contraindicated for Type 1 diabetics (even amongst fasting advocates). In fact, in spite of a deep internet search, I could only find one account of a type 1 diabetic embarking on an extended fast (Katherine Witherell did two 14 day water fasts in 2015). As you will see from my experimentation below, I have violated all of these well known rules. To make matters worse, I even reuse my needles and stabbers. 😉
The Fasting Mimicking Diet
In 2017, a publication in the journal Cell8 swept the diabetes world with the words “Reverse Diabetes” in the title. There are thousands of such articles that claim to reverse diabetes. Many are related to type 2 diabetes (and probably do in fact help). In contrast, the situations where type 1 diabetes has been reversed either require a pancreas transplant (with accompanying life-time immunosuppressants) or they are preliminary results from some unobtanium compound that has only been tested in mice – further research required.
At first glance, I was appalled by this so-called Fasting Mimicking Diet – largely because the head researcher, Valter Longo, had started a company selling a FMD product. Seems too fishy to me: basically get a research paper published to promote your products. Moreover, the primary experiment was in mice (though they also experimented with human pancreatic beta cells in culture). Finally, the mouse model that they used for type 1 diabetes isn’t the same as what is going on in human diabetes. The mouse pancreases have been poisoned (a one time event), whereas in human type 1 diabetes, the immune system is presumably constantly attacking the pancreas. For those reasons, I shunned the paper.
But I couldn’t help but be intrigued by the data, and spent a lot of time reading the paper, and looking carefully at the results. The claim is that using repeated cycles of the Fasting Mimicking Diet (FMD), mice were able to restore their pancreatic beta cells. Digging into the data, I found that actually only some of the mice succeeded in doing this after 50 days – about half of them. Nevertheless, I figured that I could adopt my own version of the FMD and give it a go. The pre-packaged food from that website costs $300 for a few days. I investigated the macronutrient composition, and the theory behind how it worked, and realized that the main goal is to restrict protein. The official FMD is about 700 calories per day in humans. I decided that I’d try and keep my daily calories as far under that as comfortable (to get as close to water fasting as possible). Also, I made sure that anything I did eat had negligible amounts of protein. This plan wouldn’t cost anything, but it was risky; I would be extraordinarily careful by testing my blood glucose often, and I could stop at any time. I decided it was worth it because besides the possible positive impact on my dead beta cells, fasting may have other health benefits as well.9
In the 2 weeks leading up to the start of this first cycle, I practiced skipping breakfast and not eating until noon. I also did a few days where I only ate one meal (an early dinner around 5pm). Not only did this pattern change make it easier to transition into the FMD, but it actually had a big impact on reducing my insulin needs. I continued my exercise during this time, which happened to be an 8 day tour through Southern California. (about 6 hours of endurance bike riding per day).
The Results
Let’s begin with a compilation of the macronutrients for each day:
| Day Number | Calories | Digestable Carb (grams) | Protein (grams) | Fat (grams) | Calories Burned (according to Strava) |
|---|---|---|---|---|---|
| 1 | 281 | 24 | 3 | 21 | 1418 |
| 2 | 313 | 5 | 4 | 26 | 0 |
| 3 | 358 | 3 | 4 | 32 | 717 |
| 4 | 384 | 6 | 4 | 35 | 288 |
Below is the direct data from myfitnesspal. Note that I did not record zero-calorie items in myfitnesspal (perhaps I will next time). Zero calorie items I consumed were 1) Black Coffee on days 1-3 of the fast. 2) Pink Himalayan salt – about 2 tsp each day. 3) Water 4) Two cups of black tea on day 1 or 2 – can’t remember 5) Mint tea on day 4.
- Day 1, June 21 Food Diary: 24g net carb, 3g protein, 21g fat, 281 calories
- Day 2, June 22 Food Diary: 5g net carb, 4g protein, 26g fat, 313 calories
- Day3, June 23 Food Diary: 3g net carb, 4g protein, 32g fat, 358 calories
- Day 4, June 24 Food Diary: 6g net carb, 4g protein, 35g fat, 384 calories
Here is what my blood glucose reading were in chart form:
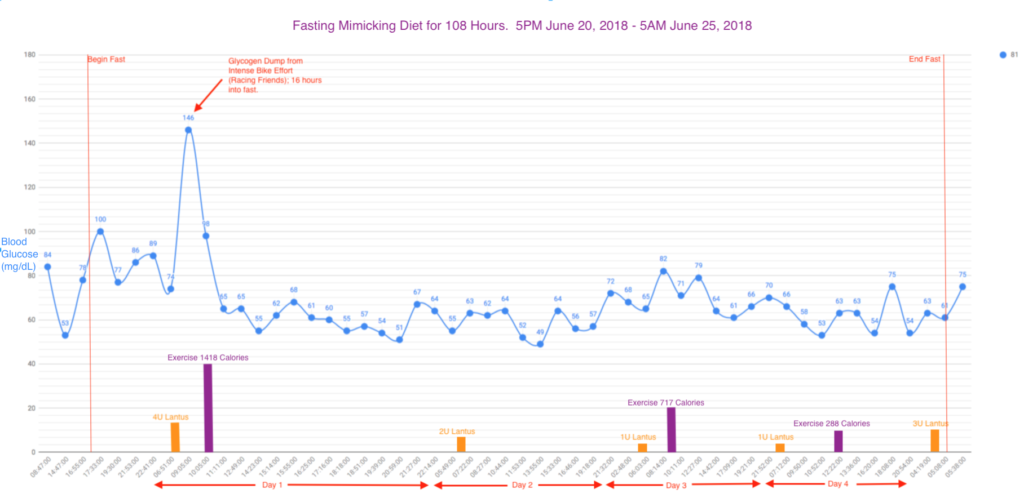
The results during the first cycle of a 4.5 day utilization of my version of a Fasting mimicking diet in a person with type 1 diabetes. The Y-axis is my blood glucose in mg/dL. I have indicated exercise in purple (calories were determined from my Strava account), and insulin dosing in orange. I only took Lantus during this period, as using any Novolog would have certainly been too much.
You may be wondering about those all those readings in the 50s.. and one in the 40s! Prior to adopting this diet, I would have severe symptomatic hypoglycemia when my blood sugar dipped below 60mg/dL. I’ve even felt hypoglycemic in the 80s on certain occasions, though never severe. In my research, I found several accounts of NON DIABETICS tracking their sugars during a fast – and these guys would often be in the 50s.101112 I figured that if a non-diabetic can do fine with glucose in the 30’s, I might be able to carefully pull it off. Remember, this page is not medical advice, nor do I endorse this for others. This is certainly very risky – so I proceeded with extreme caution – testing frequently and assessing how I felt the entire time. I also had reduced my insulin so significantly, that I figured that if anything, I’d develop high blood sugars and ketoacidosis. As an additional precautionary measure, I took urine ketone readings periodically – just to ensure that I wasn’t in an unusual state of ketotic hypoglycemia. Urine ketones were always measured as “small” (15mg/dL). I’m not reporting the detailed data because I did it irregularly and because urine test strips only show part of the picture (Mine only measure Acetoacetic acid – just one of the 3 ketone bodies expected to be present… and presumably your body is using the ketones for fuel as opposed to excreting them).
Besides the glucose, my second most significant observation is that I had a dramatic decrease in blood pressure throughout the experiment. Here are two snapshots of my blood pressure (plus a non-fasting baseline at top):
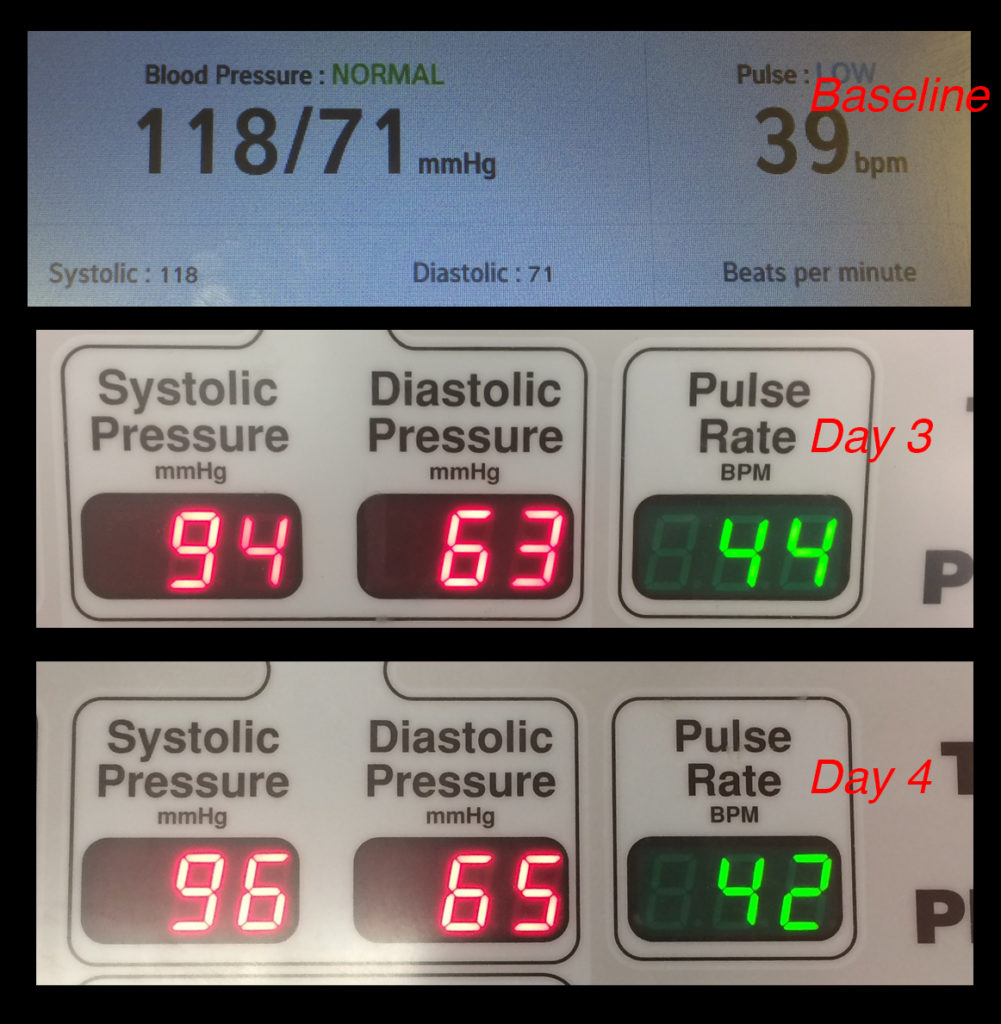
This thumbnail reminds me of the dashboard on the Back To The Future car! The biggest symptom I had from fasting was dramatically reduced blood pressure. I consumed about 2 tsp of salt per day in an attempt to maintain blood pressure. In spite of that, I experienced frequent episodes of postural hypotension where I had to be very careful not to stand up too quickly or risk blacking out. Also, presumably as a result of the reduced blood pressure, I’d easily get “pins and needles” in my hands and arms.
What I find fascinating is that I was able to survive on 1U of Lantus for 2 days, and never once have a high blood sugar (if you don’t know, overnight fasting blood sugar should be between 70 and 100 in a non diabetic). This means that by 11am on day 1, thanks partly to my exercise and having fasted since 5PM the day before, my blood sugars – as a type 1 diabetic – were actually below normal with very little insulin.
How was the Fast?
Non-diabetics who write about fasting often give a detailed blow-by-blow discussion of how they felt during the fast, and I pretty much felt the same way. I felt weak at the end of day 1, and into day 2. Felt great on day 3 and was getting pretty hungry by the night of day 4. On my next cycle, I may start eating on the night of day 4 instead of pushing it to the 5th day like I did this time. One observation was that I was in a really good mood and felt happy and relaxed about life. Maybe I was just extra happy because I felt like everything was going so well – but I really had a feeling of levity and brightness towards the world. I was astonished that I could go this many days with so little insulin. Having the knowledge that I can survive without much food or insulin – and continue to exercise – is extremely liberating. I do a lot of backpacking and biking in remote locations – places that are often days of exercise away from food (and even longer away from insulin supply)! Knowing that I can keep exercising without insulin (as long as I don’t eat) is a huge weight off of my shoulders. I do often worry about losing my insulin, having it stolen, having the pen break, or having it stop working due to the temperature extremes that I travel in.
Next Steps
I’m already eager to try this again! But – I need to wait. If there is any hope for this project to partially restore my beta cells, the restoration would happen during the re-feeding phase, not the fasting phase. In other words, this is just like training for bike racing: You break yourself down with a hard workout, and then you build yourself up with food and rest. So that’s what I’m doing: Refueling carefully with foods that are very high in nutrient content. Almost all of the abundant produce is from our backyard garden which sees neither herbicides nor pesticides. For added recovery, I’m pulling the plug on coffee and alcohol indefinitely. Alcohol is known to damage the pancreas13, so to give these cells their best chance at healing, I’m stopping. In the past, I’d take advantage of the slight blood glucose lowering effects of a glass of wine. Here is the re-feed food (note that myfitnesspal takes calories from Strava, but tends to over-estimate towards my calorie goal).
- The Re-Feed
- The Re-Feed
- The Re-Feed
Lastly, I’m always frustrated when I encounter blog posts where someone has conducted an experiment, and they promise to follow up. My intention is to follow up long term with the progress of this experiment in future posts. I do plan to execute at least two more sessions of the fasting protocol. The regime is that you conduct the fast 5 days every month, though I’m sure that it is very flexible. I don’t expect to see any results from this particular cycle – in the mice it wasn’t until about day 30 that changes to blood glucose were seen (and the mice were on a tighter schedule of 4 days Fasting, 7 days re-feeding). My doctor did agree to schedule a c-peptide test for my curiosity, so that is also forthcoming. To be fair, I plan to take that test “stimulated” which means that I will briefly challenge my pancreas with some glucose (for which I don’t inject insulin) shortly before the test. Stay tuned; Results from cycle 2 of the FMD will be posted here.
References
- Caroline’s Story: Overcoming Type 1 Diabetes with Real Food – Caroline Potter eliminates insulin for 2.5 years by changing her diet. Eventually, she does need to resume insulin
- PreventT1D.org #WeAreNotWaiting for definitive research studies when we can safely take action now to improve our odds.
- Törn C, 2003, C-peptide and autoimmune markers in diabetes. https://www.ncbi.nlm.nih.gov/pubmed/12593469
- David M. Tridgell, Charles Spiekerman, Richard S. Wang, and Carla J. Greenbaum, 2011, Interaction of Onset and Duration of Diabetes on the Percent of GAD and IA-2 Antibody–Positive Subjects in the Type 1 Diabetes Genetics Consortium Database https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3064062/
- COSIMO GIANNINI, MD1 NICOLA SANTORO, MD, PHD1 SONIA CAPRIO, MD1, GRACE KIM, MD1, DEREK LARTAUD, MA1 MELISSA SHAW, MA1 BRIDGET PIERPONT, MA1 RAM WEISS, MD, PHD The Triglyceride-to-HDL Cholesterol Ratio http://care.diabetesjournals.org/content/diacare/34/8/1869.full.pdf
- There are many other challenges which I’m not going into detail on, including the extremely high cost of insulin analogs, the difficulty in obtaining insulin in remote locations including the 3rd world, Insulin concentrations being formulated for type 2 diabetics as opposed to endurance athletes, the difficulty in keeping your insulin above freezing and below 80F, etc. I plan to discuss these challenges and ways to overcome them in a future post.
- Northampton man with type 1 diabetes who stopped injecting says he has rare gene
- Chia-Wei Cheng, Valentina Villani, Roberta Buono7, Min Wei, Sanjeev Kumar, Omer H. Yilmaz, Pinchas Cohen, Julie B. Sneddon, Laura Perin, Valter D. Longo, 2017, Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes https://www.cell.com/cell/fulltext/S0092-8674(17)30130-7 (February 23, 2017)
- Michelle Harvie and Anthony Howell, 2017, Potential Benefits and Harms of Intermittent Energy Restriction and Intermittent Fasting Amongst Obese, Overweight and Normal Weight Subjects—A Narrative Review of Human and Animal Evidence https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5371748/
- W. K. Stewart and Laura W. Fleming, 1973, Features of a successful therapeutic fast of 382 days’ duration https://idmprogram.com/fasting-physiology-part-ii/
- During his Fast, Quantified Bob had readings of 55, 44, 53
- Damien Blenkinsopp had glucose reading dip below 60 mg/dL often during his 10 day fast.
- Marta Herreros-Villanueva, Elizabeth Hijona, Jesus Maria Bañales, Angel Cosme, and Luis Bujanda, 2013, Alcohol consumption on pancreatic diseases https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3574589/







































Hi Brian I was wondering if this ultimately ended up working for you?
Hi Chloe – Thank you for your question. I don’t know if you read my post on Cycle 2 (if not you may want to because I include some more resources)… But to summarize: No, it did not work. When I started, I thought that I was pioneering this type of experiment in humans – but then I found a group (which I linked to in part 2)… and several of them had tried it with no improvement in c-peptide that you could absolutely attribute to the diet. Some people went in to have their c-peptide tested frequently, and it seemed as if the changes in their c-peptide were not related to the FMD in that they would go up and down. No one seemed to get a c-peptide level that was adequate to stop or reduce insulin needs. Maybe I gave up too soon? I’d be willing to do something difficult and challenging if I felt like it would be helpful – but in the end, I would say that this diet was more detrimental than beneficial. I say that because once you end the diet, you quickly go back to needing just as much insulin – or even more – than you did pre-diet. Diabetes is unstable enough without adding in the complexity of irregular fasting.
Hello Brian.
Big respect for you to be on such path only three years after the diagnosis!
I’d love to be in contact with you and pick your brain about FMD and your active life with T1D,
Cheers
Gil