When is a carb not a carb? The great fructose experiment.
All material on this website is provided for your information only and may not be construed as medical advice or instruction. No action or inaction should be taken based solely on the contents of this information; instead, readers should consult appropriate health professionals on any matter relating to their health and well-being.
By 2019, you’ve probably heard someone claim at one point that “sugar is bad.” Many people don’t even know what “sugar” is, so this blog post is going to attempt to teach some “sugar science.” First, I’ll do some basic chemistry regarding sugar, and finally, I’ll take you to my own personal experiment that is relevant to people with type 1 diabetes. If you think you already know the sugar science and just want to skip to the experiment, click here.
What is Sugar?
First, we must define sugar. If you’re like most people, you imagine “table sugar” when you hear the word. In fact, many think that table sugar is the only sugar. It turns out, that table sugar is actually a combination of two other sugars in a 50/50 ratio: glucose + fructose.
What is sugar? When most people think of sugar, they imagine “table sugar” which is made of sucrose molecules.
Now that you think about it, you’ve probably already heard of glucose, fructose, and sucrose. In fact, you’ve probably already heard of lactose too. Notice anything in common between these words? They all end in “-ose“. In chemistry, the “-ose” ending means a molecule is a sugar. This rule works really well with chemistry, but not so well with other words that end in “-ose” such as “nose” or “panty hose“. Neither one of those will give you a sweet taste in your mouth.
In natural foods, you’ll most commonly encounter the following sugars:
- Glucose (GL)
- Fructose (FR)
- Galactose (GA)
Those 3 sugars (called “monosaccharides”) make up the backbones of two other sugars you have probably already heard of as well:
- Sucrose (GL + FR)
- Lactose (GA + GL)
Notice how in the 2nd list that Sucrose is a combination of GL + FR. That means that a Sucrose molecule (table sugar) actually consists of one Glucose and one Fructose bound together. When two monosaccharides are bound together (see my first list), they become a disaccharide. And those monosaccharides can combine into longer molecules such as amylose, which looks like this: (GL + GL + GL + GL + GL + GL + GL……….). Because it is a long chain of sugars, amylose is called an oligosaccharide. Now, to Review:
- saccharide means “sugar”
- Mono means “one”
- Di means “two”
- Oligo means “many”
Notice the pattern here… amylose ends in “-ose” making it a “sugar”.. and it is just a long chain of one of the 3 basic sugars mentioned above… glucose. Since it is a chain of many glucose molecules, is called an “oligosaccharide”.
In food, we tend to call the monosaccharides and disaccharides “sugar.” Most of these molecules taste sweet (to varying degrees). But look at amylose above: it’s a long chain of sweet sugars (Glucose)…. but it doesn’t taste sweet at all. How do I know? Because a regular potato isn’t sweet, and it’s 20% amylose! So a food like potato is chock full of these sugar molecules, but they don’t taste sweet like sugar because they are long chains of sugar instead of individual molecules, and your tastebuds can’t sense the chains… only the smaller sugar components. But just because you can’t taste it doesn’t mean the sugar isn’t in the potato!
Other examples of foods with long chains of sugars are bread, pasta, maltodextrin, etc.. These foods are often called “high carbohydrate” foods. They don’t taste sweet, but they are effectively made mostly of sugar joined into long chains. Once you eat these items, your digestive enzymes VERY QUICKLY (like in seconds) break the long chains of sugar into their simpler components. Effectively, there is not a very big difference in your body (sugar-wise) between consuming a slice of white bread or eating a handful of sugar tablets! This is why a hamburger bun can send blood sugar skyrocketing – even though it doesn’t taste sweet at all.1
So, what do we call these longer chains of sugar that don’t taste sweet? On an American Nutrition Label, we lump the sweet tasting sugars along with the long chain “sugars” into one term: Carbohydrate. On that label, you will often see “Carbohydrates” and as a sub-set of Carbohydrates, you will see “sugars”. Also, as a subset of Carbohydrate, you will see “Fiber.” Fiber is the portion of carbohydrates that generally cannot be digested by your digestive enzymes, so in some cases, diabetics will subtract fiber from the total carbohydrate content.2
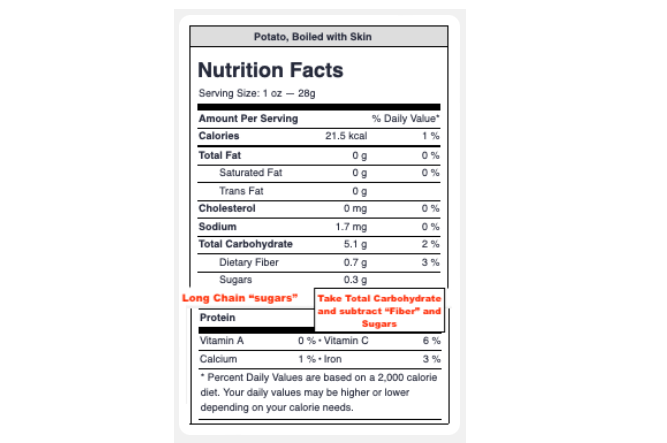
Although American Food Labels only include two line items for total carbohydrate, carbohydrate is composed of 3 broad groups: 1) Fiber – this consists of the generally non-digestible carbohydrates. 2) Sugars – this consists of the simple sugars that we discussed above (monosaccharides and disaccharides). 3) Everything else… (oligosaccharides). The 3rd item is simply calculated by taking the total carbohydrate (in this case 5.1g) and subtracting the fiber (0.7g) and the sugar (0.3g). This means you’re left with 4.1g of oligosaccharides that are digestible and will rapidly convert to sugars once consumed.
Now that you know more about the different types of sugar, let’s learn a little more about what we are actually measuring when we “check our sugars” with a meter…
What are we measuring when we “check our sugars?”
If you have diabetes (or even if you don’t), you probably know that diabetics “check their sugars.” They have a small device called a “glucometer” that lets them know the concentration of sugar in their blood. You may have figured it out by now because there is a hint in the name “glucometer”…. these meters are sensitive to only one of the many sugars mentioned above: Glucose. That means that if there is lots of galactose or fructose in your blood, the meter won’t show it; the meter only reads glucose. The reason a glucometer is useful is because almost all of the sugars mentioned above quickly turn into glucose. For example, galactose is quickly turned to glucose in the liver. Many of the oligosaccharides in bread, potatoes, and pasta (remember the GL + GL + GL + GL + GL……. molecules mentioned above!?)… all those get swiftly converted to GL… glucose. This means that a glucometer is effectively able to measure all of the sugar in the blood.
But you may have noticed that I didn’t mention a couple of the simple sugars from the first list…. I didn’t mention “sucrose” (which is table sugar), nor did I mention “fructose”…
What about Fructose?
It turns out that unlike glucose based carbohydrates, fructose can experience a number of fates in the human body. When it comes to fructose, it’s kind of like a choose your own adventure. Here are some of the possible fates:3
- Fructose can be poorly absorbed by the intestines, so the body never “sees” it…
- Fructose can be “burned” to make ATP/CO2 (in liver, intestine, kidney, fat, and muscle)4
- Fructose can be converted to fat, glycerol, and glycogen.
- Fructose can be converted to glucose (this is the only case where you’d see it on your glucometer)
It’s important to remember that table sugar (sucrose) is 50% fructose. So if you eat a “spoonful of (table) sugar”, you’re actually taking in half a spoonful of glucose and half a spoonful of fructose. We know that your glucometer will tell you how much glucose you just ate, but given the variegated and mysterious fates of fructose listed above – plus the fact that your meter cannot register fructose, means that you may be able to consume fructose and not see a spike in your blood sugars – or need to dose insulin for said fructose. At the bottom of this post, I will discuss the implications of this.
The Experiment
The experiment is this: I will consume 14g (or 0.5oz) of pure fructose which I purchased from the health food store. If I ate this much glucose, I’d need to inject 2U of insulin to keep my blood sugar stable… and if I didn’t do that, I could expect to see my blood glucose rise by > 70mg/dL
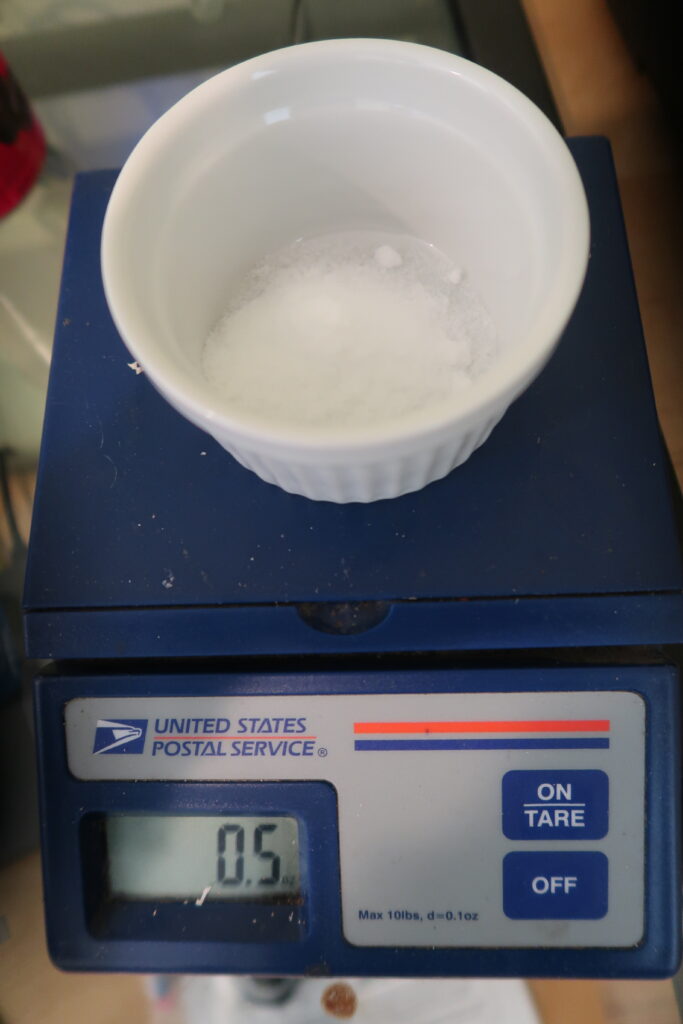
Here is the fructose. I will consume 14g (0.5oz) of powdered fructose. I will not inject any insulin for this experiment. If the blood glucose rises, this means that the fructose in my body was converted to glucose (one of the many possible fates of fructose). Note that if I ate the same amount of glucose, it would raise my blood sugar by 70 points – which would be very clearly seen on the glucometer. Also, to compensate for this much glucose I would ordinarily need to inject 2U of insulin.
Although I cannot perform my own isotopic tracer experiment to see what happens to fructose when I eat it, I do have an experimental advantage of being a type 1 diabetic. As a type 1 diabetic, I know exactly how much insulin is in my body – because I’m the one who puts it there! For a non-diabetic, an experiment like this would not work because it would be impossible to know the effect of the fructose because the healthy pancreas would respond by making insulin so the fructose could “disappear” into the cells – never being measured by the glucometer. In my case, I will not inject any insulin for the fructose.

This is what the mass-equivalent dose of glucose tabs looks like. If you have diabetes, you probably know that this many glucose tablets would send you SKY HIGH if you didn’t inject insulin along with it. Let’s see what happens when I consume this much fructose instead…
So, here is what the results of eating purified fructose with no extra insulin on board look like:

The experiment began at 10:14am, and lasted 1 hour until 11:16am. Before beginning the experiment, I was fasted all night, and had stable blood sugars ~80 for the 3 hours leading up to the experiment. During the experiment, I just sat at my desk and performed no exercise (which could theoretically burn some glucose making it “disappear”). Note that if I had ingested the equivalent dose of glucose tablets, my readings would easily be greater than 160mg/dL.
As you can see from the results above, eating pure fructose did NOT make my blood glucose meter budge. Yes, I got a reading of 87, but keep in mind that this is within the accuracy range of this meter; also even if it is real, that’s an insignificant jump compared to the expected 160mg/dL had I consumed glucose. So, what happened here?
What happened to the fructose?
The unfortunate answer is: I don’t know. Maybe the fructose wasn’t absorbed by my gut, and just got fermented by the bacteria living there. Maybe the fructose did get absorbed. If so, because the meter cannot measure fructose, its presence in the blood was not displayed. But what about the 3 other possible fates for fructose mentioned above (burned directly, converted to fat, converted to glucose)? Of those 3, the only one we can be sure about is the last one: In my body, fructose was not converted to glucose and distributed through the bloodstream. You may be disappointed to learn that this is about all we can conclude from this experiment. But keep reading to see why this experiment is still important for type 1 diabetics, type 2 diabetics, and even healthy people…
Why does this matter?
For diabetics who are dosing insulin, this is very important. Almost every fruit contains about 50% glucose and 50% fructose. Some fruits contain sucrose, but as you learned above – sucrose itself is 50/50 glucose fructose anyway – so the 50/50 rule still holds true. As you can see from my experiment, no insulin is needed for the fructose. In fact, if I had taken 2 units of insulin for these 14g of carbohydrate, I’d be dealing with some serious – even dangerous hypoglycemia. For example, let say I’m going to eat a small apple which has 14g of carbohydrate. I know that my insulin to carb ratio is 1:75 – so if I take the 14g of carbohydrate in the apple and divide it by 7 from my 1:7 I:C ratio, I get 2. 2 is the number of units of insulin I would need to inject. But, because of this fructose phenomenon, I should REALLY only inject 1U. Why? Because half of that carbohydrate is fructose – and I don’t need any insulin for the fructose. This is very important because if I inject too much insulin, I’ll get hypoglycemia (athletes will kind-of recognize this feeling as “the bonk” – except this is much worse).
Meanwhile, if I eat a slice of white bread – even though the label says it has 1g of sugar (but 14g of total carb) – I’ll need to inject 2U because the bread contains 1g of glucose… and 13g of oligosaccharides – all of which convert into glucose.
Hopefully you can see from this small example that an insulin to carb ratio alone cannot dictate how much insulin you need for a certain foodstuff. In fact, there is WAY more nuance than this – involving lots of different types of sugars that I didn’t discuss in this post (like allulose, maltose, etc.)… and also the various types of protein (which have different ratios of their sub-components called amino acids). Finally, fatty come in all shapes and sizes varying from the small “Acetic acid” up to the large “Stearic acid” – and many different fatty acids in between. Each of these fatty acids and amino acids have different effects on blood sugars (and thus insulin dosing) which I hope to address in a more advanced-level post in the future.
So is fructose a “free” sugar?
You may have postulated by now that if fructose doesn’t make the blood sugar meter move, it’s a “free sugar” – just like other non nutritive sweeteners like aspartame, stevia, and erythritol.
My answer to this is: probably not. If you pay attention to nutritional news at all, you have probably been warned that fructose “turns into fat”. Although my experiment doesn’t prove this, we can see that the fructose definitely did not take the Fructose->Glucose pathway… meaning that it may have gone down the Fructose->Triglyceride (fat) pathway. A large quantity of research exists on this topic, so I’ll just summarize the research that I think might be true:
- Fructose can optionally be converted to Triglycerides (fat) through fructolysis/lipogenesis. (see papers and discussion above).
- The intestine, kidney, adipose tissue, and muscle have limited capacity to use fructose, so UNLESS YOU’RE ACTIVELY EXERCISING (which will use up fructose quickly instead of sending it to the liver),6 the excess fructose must be dealt with by other organs; primarily the liver.
- The liver itself has a limited capacity to process fructose,7 and if fructose exceeds this capacity, it can lead to non-alcoholic fatty liver disease
- Non-alcoholic fatty liver disease is something you don’t want.8
Based on just that information alone, even though fructose doesn’t move my glucose meter or require insulin, my decision has been to keep my fructose consumption low. If I’m being sedentary, I’ll limit fructose to the amount found in a piece of low-sugar fruit. That could be a small apple or a small bowl of strawberries or raspberries. Also, from the research (see my references above), it seems that the muscles can use fructose if you’re actively exercising – this should help bypass the toxic effects on the liver because the liver does not need to “clean up” excess fructose floating around. Therefore, I have also used larger portions of fruit during longer bike rides under the assumption that my muscles will use the fructose before it can be stored by the liver. In my research, I cannot find evidence that small amounts of fructose are problematic in sedentary people. The cut-off according to this diagram seems to be 11mg/dL. If you weigh 165 pounds, you would achieve that blood concentration of fructose with one small apple.
The above addresses the “traditional” concerns of fructose – but there is actually something even worse about fructose that makes me as a type 1 diabetic even more wary of its consumption.
Fructose and glycation
If you have diabetes, you’re probably very familiar with the HbA1c test. This measures the level of glycation (carbohydrate stuck to biomolecules – in this case proteins – in your red blood cells). This same process isn’t limited to proteins; fats and even DNA can also undergo this chemical modification. As a diabetic, when you’re aiming for a lower A1c, essentially you are trying to reduce the amount of glycation going on in your body. The reason for this is because it is well established that advanced glycation end products are the primary contributor to diabetic complications.9 Why am I bringing this up? Because I read that fructose is 8-10 times more reactive than glucose in the formation of advanced glycation end products. 10 If that is true, then I think it is safe to say that even though fructose may not be showing up on our meters, the most prudent move would be to try and avoid it except in small quantities during exercise.
P.S.
I started writing this post Oct 15, 2019 and finally got to publishing it in August 2023! I’ve got a lot more for you, but it takes a long time to do my research…
References & Footnotes
- Note: I know I mentioned “amylose” as a sugar. The human body does not have enzymes to break down amylose into its simpler components of glucose; instead it is fermented by gut bacteria. The reason I used amylose as an example from a potato is because it helps simplify the “-ose” theme. Potatoes also have amylopectin, which IS able to be quickly broken down by digestive enzymes. For the sake of simplicity, I’m avoiding mentioning it in the primary text of the blog post.
- Note: Fiber is very nuanced, and often not recorded correctly on American Nutrition Labels. For example: A potato is 11%-20% amylose, which your digestive enzymes cannot digest. BUT the bacteria in your stomach may or may not be able to ferment the amylose. If they do ferment it, they will effectively convert it to fat (short chain fatty acids to be exact). This gets really complicated because there are MANY different types of fiber, and although these fibers generally cannot be digested by humans, there is a great diversity of microbes in our guts. The end result is that every person will get something different from fiber – making it very difficult to describe the fate of these molecules in absolute terms. For dosing insulin, most diabetics tend to subtract out the fiber content of a meal when estimating their dosage – but everyone is going to be different. Some people need to include fiber as part of their insulin calculation because their personal gut flora enables them to (effectively) absorb energy from the fiber.
- Reference: Fructose metabolism in humans – what isotopic tracer studies tell us, Sam Z Sun, 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3533803/
- Reference: Biochemistry, Fructose Metabolism, Sagar J. Dholariya et al, 2018, https://www.ncbi.nlm.nih.gov/books/NBK576428/
- Note: For non-diabetics, an insulin to carb ratio (or I:C) is a personal number that you use to calculate how much insulin you need for every gram of carbohydrate. This number can vary significantly amongst individuals, and it can even vary within the same individual based on the time of day or how much exercise they have been doing lately, or how much fat they have been eating lately. Most diabetics will know *approximately* what their I:C ratio is, and they will use it to estimate a safe but useful amount of insulin to inject before each meal.
- Reference: Exercise performed immediately after fructose ingestion enhances fructose oxidation and suppresses fructose storage, Léonie Egli et al., 2015, https://pubmed.ncbi.nlm.nih.gov/26702120/
- Reference: Fructose Consumption, Lipogenesis, and Non-Alcoholic Fatty Liver Disease, Kasper W. ter Horst and Mireille J. Serlie, 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5622741/
- Reference: Mortality in biopsy-confirmed nonalcoholic fatty liver disease: results from a nationwide cohort, Tracey G Simon et al., 2021, https://pubmed.ncbi.nlm.nih.gov/33037056/
- Reference: Advanced Glycation End Products and Diabetic Complications, Singh VP, Bali A, Singh N, Jaggi AS., 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3951818/
- Reference: Formation of Fructose-Mediated Advanced Glycation End Products and Their Roles in Metabolic and Inflammatory Diseases, Alejandro Gugliucci, 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227984/



























Thank you, Brian, for explaining much of the mystery so clearly.
Peter Attia’s podcast had a deep dive into fructose. Might be worth a listen if you have 2 hours. https://peterattiamd.com/rickjohnson2/
Brian – Glad to know that you listen to Peter Attia. I do to, and have listened to all of his episodes involving metabolism… even the stuff related to type 2 diabetes, which I do not have. Thanks for mentioning Peter; he is one of my favorite podcasters. So thorough.
Wow Brian! This is really interesting information. I knew the basic information regarding glucose/white sugar and fructose/fruit sugar and how the body converts various foods to glucose/sugar. I had no idea what a huge load on the liver fructose could have! Now that we are aging and don’t exercise to the extent we used to that’s pretty thought provoking!